
This is also discussed in the rhythmic activity section of the epileptiform activity page.
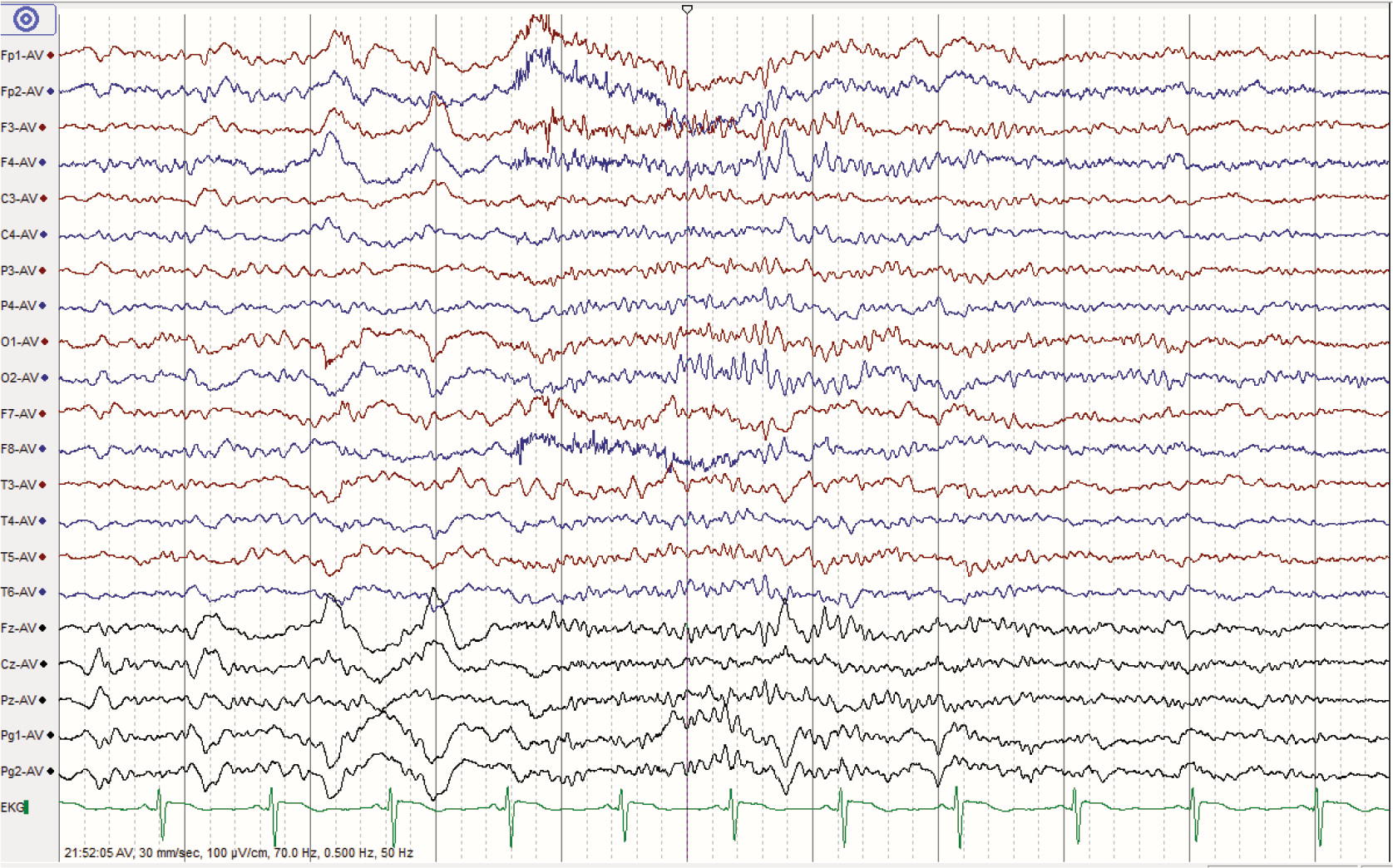
In order to be categorized as rhythmic activity, there must be 6 cycles of the activity for example, one wave per second for 6 seconds, or two waves per second for 3 seconds. When focal slowing is seen as intermittent rhythmic delta activity, its significance varies by the region of the brain involved, with some locations suggesting epileptic potential and others just nonspecific encephalopathy. On the example below, note how the left hemisphere (maximal temporally) continuously has a slower to at times absent PDR compared to the right, and is marked by theta to delta activity while the right hemisphere has normal alpha and beta activity. Intermittent focal slowing can also arise due to a structural abnormality, but such abnormalities tend to be smaller in nature, such as a focal cortical dysplasia or the beginnings of a small tumor, and thus are more likely seen on EEG with certain state changes, overlying illness, or medication effect (this is not a hard and fast rule). While slower frequencies (delta vs theta, for instance) don't necessarily suggest a worse underlying abnormality, continuous slowing is worse than intermittent, and a rule of thumb is that the less reactive and variable a slowed region is, the worse the underlying cerebral dysfunction. Continuous/persistent focal slowing is suggestive of a significant structural abnormality such as tumor, bleed, ischemic infarct or demyelinating lesion. Polymorphic slowing is most commonly seen and is thought to arise from a mix of white and grey matter injury but is generally nonspecific in etiology, while monomorphic/rhythmic slowing is thought to localize more to grey matter but, more importantly, is often concerning for epileptiform activity. When considering any slowing, break it down into being either Slowing can be either continuous or intermittent and either polymorphic or monomorphic/rhythmic. Intermittent slowing can also be any of these things, but more often suggests a smaller lesion such as focal cortical dysplasia or the beginnings of a small tumor, and thus is more likely seen on EEG with certain state changes, overlying illness, or medication effect (this is not a hard and fast rule). Continuous slowing is suspicious for a larger lesion such as a tumor, bleed, ischemic infarct or demyelinating lesion. First, it can be persistent/continuous or intermittent. While generalized slowing suggests diffuse brain dysfunction, focal slowing is typically evidence of a structural abnormality involving the slowed area, particularly if the slowing is mostly delta. Severe generalized slowing is highly disorganized and often discontinuous without reactivity or appreciable architecture such as an AP gradient or PDR, and is usually predominated by low amplitude delta activity.

With moderate generalized slowing the PDR is very fragmented or gone entirely, and the record is often predominantly theta into delta activity with much less alpha. Mild generalized slowing is typically marked by the presence of a slowed PDR and a poor AP gradient, often with excess theta admixed with the normal alpha activity throughout reactivity, variability and the other markers of a normal awake EEG remain. The exact delineation from one to the next is somewhat subjective, but a few rules of thumb may help. Generalized slowing can be categorized into mild, moderate and severe. Disorganization goes in hand with generalized slowing, a nonspecific finding suggestive of diffuse cerebral dysfunction / encephalopathy as can be seen with severe infections, medication or substance abuse, or neurodegenerative disease. If any of these things are lacking in a tracing, it is said to be disorganized. Recall that when reading the background, you should look for a clear PDR, AP gradient, synchrony, symmetry, continuity, reactivity, and clear wave morphology.


 0 kommentar(er)
0 kommentar(er)
